What is a Disc Bulge or Herniated Disc and are they the same thing?
A bulging disc is like letting air out of a car tire. The disc sags and looks like it is bulging outward. This is typically considered the first of 4 stages of a herniated disc. With a herniated disc, the outer covering of the disc can progress to have a hole or tear. This causes the nucleus pulposus (jelly-like center of the disc) to leak into the spinal canal and can push on the nerve causing symptoms in the lower back all the way down to the toes.

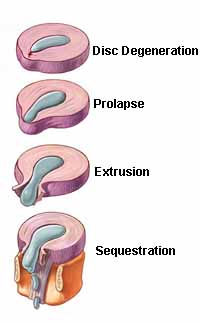
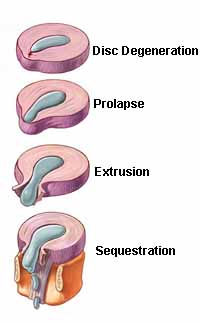
Differentiate different stages of injury
There are 4 stages of disc herniation.
- Disc degeneration
- Disc prolapse
- Disc extrusion
- Disc Sequestration
How Did I Get a Herniated Disc?
Although some people will experience a single traumatic event involving excessive strain and/or compression of the disc, disc herniations are most often associated with gradual and progressive degeneration.


Symptoms of a Herniated Disc
Symptoms of a herniated disc may include, but are not limited to:
- Lower back pain
- Pain that worsens with movement (particularly forward bending)
- Pain that can be worse with sitting.
- Nerve pain (sharp, searing, electrical shock like symptoms that can radiate down the leg).
- Foot drop – in extreme cases the nerves that innervate the muscles in the feet may get compressed causing the inability to contract the muscles and ultimately loss of control of the foot.
How is a disc herniation or bulge diagnosed?
Typically a physiotherapist or physician would conduct a thorough assessment including history of the injury, symptom profile, past medical history, and information related to your home, work and exercise life.The subjective assessment is followed by a physical exam that includes a range of motion screening, testing of the nerves exiting your lower back (that innervate the skin, muscles and reflexes), testing to look for tension in the nerves and palpation/examination of the lumbar spine.
If there is still uncertainty following the subjective and objective assessment an MRI is often considered the gold standard for diagnosis; however, this is not necessary to begin treatment and studies have shown that there are as many people with back pain/herniated discs on MRI as there are who are completely pain free. As a result physicians may wait before referring you for an MRI.




Treatment options for lumbar disc herniation or bulge
- Physical Therapy including a gentle exercise program to stabilize the spine, mobilization of the spine and modalities to relieve pain (acupuncture, heat, ice, etc.)
- Medication – generally this begins with oral medication and can progress to injections of cortisone or nerve blocks in extreme cases.
- In some cases surgery is considered.
Surgery for herniated discs:
Generally speaking most people will never need surgery for a herniated disc. They will typically recover with a combination of medication and physical therapy. However, in extreme cases surgery can be an option. Microdiscectomy is often the most common option in 90% of surgical patients. This surgery is done arthroscopically and involves removing the protruding portion of the disc. In extreme cases the disc may be removed entirely and then the two vertebrae (bones in the back) are fused together.